Revenue Cycle Management (RCM) is a crucial aspect of healthcare administration that involves managing the financial processes used by healthcare providers to track patient care episodes from registration and appointment scheduling to the final payment of a balance. Effectively, Revenue Cycle Management encompasses all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. By integrating these processes, RCM enables healthcare providers to improve their efficiency and profitability.
The complexity of the healthcare billing system makes effective RCM essential. RCM helps in reducing billing errors. It also ensures that the care providers are reimbursed timely and fully for the services they provide. Furthermore, a robust RCM system is critical for maintaining cash flow and financial stability within healthcare organizations. This allows them to continue delivering high-quality care without financial hindrance.
The Components of Revenue Cycle Management
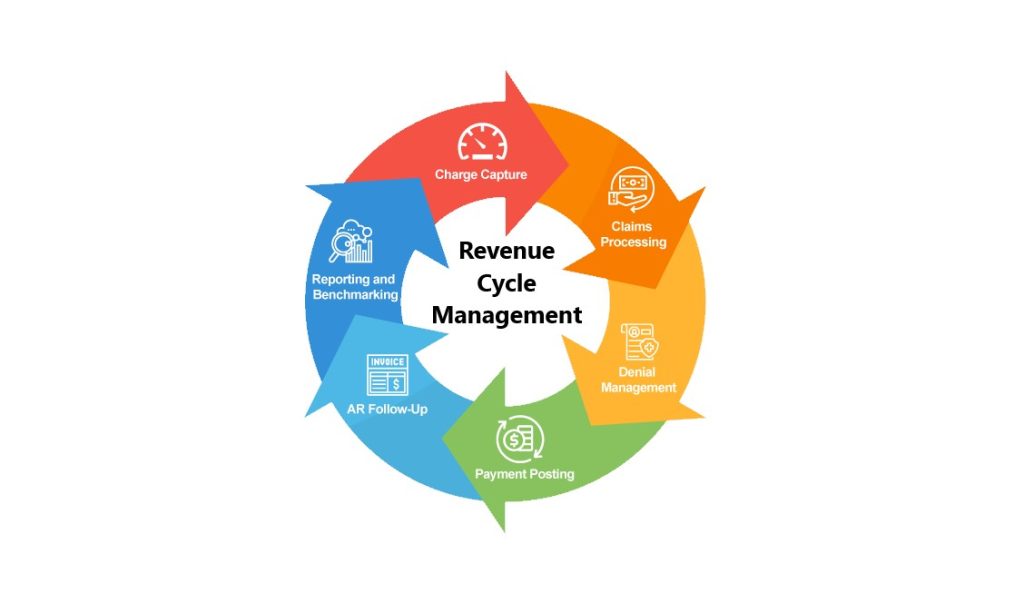
Revenue Cycle Management is a comprehensive process that begins the moment a patient makes an appointment. It continues until the account balance reaches zero. Several key components define the efficiency of RCM. They include patient registration, insurance eligibility and verification, charge capture, claim processing, payment collection, and denials management.
Each stage of Revenue Cycle Management plays a pivotal role. For instance, accurate patient registration and insurance verification can prevent delays and errors in billing. Charge capture ensures that all services provided are billed correctly. Efficient claim processing and quick resolution of denials are equally important, as they directly affect the revenue stream.
Moreover, RCM leverages technology to streamline these processes. Automated systems can handle tasks such as claim submissions and follow-ups. This not only speeds up the workflow but also minimizes errors.
Challenges in Revenue Cycle Management
Revenue Cycle Management faces several challenges that can impact a healthcare organization’s bottom line. One of the primary challenges is keeping up with the constantly changing regulations and payer requirements. This can complicate billing processes and increase the likelihood of denials. Furthermore, inadequate training of staff on the latest in billing and coding standards can lead to errors. This can delay or prevent reimbursement.
Another significant challenge is the integration of RCM software with existing clinical systems. Seamless integration is crucial for the accurate and efficient flow of information across departments. Without this, the potential for errors increases, impacting the overall efficiency of the RCM process.
Additionally, patient collections remain a hurdle. With the rise in high-deductible health plans, patients are now responsible for a larger portion of their healthcare costs, which can complicate the collections process for providers.
Best Practices in Revenue Cycle Management
To overcome these challenges, healthcare organizations must adopt best practices in RCM. First and foremost, investing in staff training and development is essential. Ensuring that all staff are knowledgeable about current billing practices, codes, and regulations can significantly reduce errors and improve the collection rates.
Additionally, healthcare providers should leverage advanced RCM software that offers robust data analysis, automated reminders for follow-ups, and efficient handling of claims and denials. Such technology not only improves accuracy but also enhances the productivity of the revenue cycle team.
Proactively managing patient responsibilities is also critical. This includes transparent communication with patients about their financial responsibilities and providing them with multiple payment options to make the process as easy as possible.
The Future of RCM
Looking forward, the role of Revenue Cycle Management is set to become even more significant. As healthcare continues to evolve, with changes in laws, patient expectations, and technology, the need for efficient Revenue Cycle Management systems will only grow. Providers who are able to adapt and update their RCM processes will not only ensure better financial outcomes but also improve patient satisfaction and engagement.
Moreover, the integration of artificial intelligence and machine learning into RCM promises to transform traditional practices. These technologies can predict patient payment behaviors, automate routine tasks, and provide advanced analytics to optimize the entire revenue cycle.
In conclusion, Revenue Cycle Management is not merely a back-office function; it is a strategic component critical to the financial and operational success of healthcare providers. Effective RCM ensures that providers are compensated timely and fully for their services, which in turn supports their mission of delivering quality patient care. As the healthcare industry continues to grow and evolve, mastering Revenue Cycle Management will remain a top priority for healthcare organizations aiming to thrive in a complex and competitive environment.